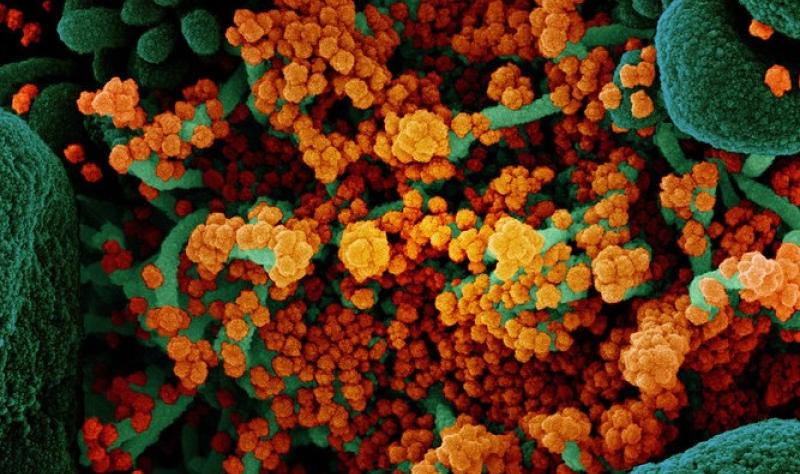
Bacterial co-infections linked to higher risk of death in US COVID patients
Although bacterial co-infections were identified infrequently in hospitalized US COVID-19 patients, they were associated with more than double the risk of death.

 Although bacterial co-infections were identified infrequently in hospitalized US COVID-19 patients, they were associated with a more than two-fold higher risk of death, US researchers reported yesterday in Influenza and Other Respiratory Viruses.
Although bacterial co-infections were identified infrequently in hospitalized US COVID-19 patients, they were associated with a more than two-fold higher risk of death, US researchers reported yesterday in Influenza and Other Respiratory Viruses.
Using data from the Coronavirus Disease 2019-Associated Hospitalization Surveillance Network (COVID-Net), which includes more than 250 acute care hospitals in 14 states, a team led by the Centers for Disease Control and Prevention (CDC) investigated the incidence of bacterial and viral co-infections among hospitalized adults with confirmed SARS-CoV-2 infections from March 2020 to April 2022. They then compared demographic and clinical features among those with and without bacterial co-infections.
Among a representative sample 36,490 hospitalized adults with COVID-19, 53.3% had bacterial cultures taken within 7 days of admission, and 6.0% had a clinically relevant bacterial pathogen in sputum, blood, deep respiratory tissue, or another sterile site.
Understanding risk factors for bacterial infections and associated outcomes can help guide clinicians in providing optimal care.
The most frequently isolated organism from all sites was Staphylococcus aureus, followed by gram-negative rods, including Pseudomonas aeruginosa, Klebsiella pneumoniae, and Escherichia coli. In-hospital death occurred in 31.7% of those with bacterial co-infections, compared with 13.2% of those without bacterial co-infections in bivariate analysis.
After controlling for demographic factors, underlying medical conditions, and time period, adults with COVID-19 who had bacterial co-infections within 7 days of admission had a relative risk [RR] of 2.28 (95% confidence interval [CI], 1.87 to 2.79) for death compared with those who had negative bacterial cultures. Those with a clinically relevant pathogen identified were also associated with an increased need for intensive care (RR, 2.11; 95% CI, 1.95 to 2.23) and mechanical ventilation (RR, 3.04; 95% CI, 2.74 to 3.37).
“As SARS-CoV-2 continues to circulate and individuals continue to be hospitalized for COVID-19, understanding risk factors for bacterial infections and associated outcomes can help guide clinicians in providing optimal care,” the study authors conclude.