Here’s what you should know about the COVID surge in Berkeley

https://assets.citysidejournalism.org/m/753d2b268a155216/large-iHealth-COVID-19-Antigen-Rapid-Tests-4.jpg
” data-image-caption=”
An iHealth COVID-19 rapid-testing kit.
” data-medium-file=”https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934-360×240.jpg” data-large-file=”https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934-1200×800.jpg” width=”1200″ height=”800″ src=”https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934-1200×800.jpg” alt class=”wp-image-461619″ srcset=”https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934-1200×800.jpg 1200w, https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934-360×240.jpg 360w, https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934-200×133.jpg 200w, https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934-768×512.jpg 768w, https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934-1536×1024.jpg 1536w, https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934-720×480.jpg 720w, https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934-480×320.jpg 480w, https://www.berkeleyside.org/wp-content/uploads/2022/07/20220517-211934.jpg 1600w” sizes=”(max-width: 1200px) 100vw, 1200px”>
The COVID-19 surge in Alameda County that began in May has continued into late July, driven by a highly transmissible sub-variant called BA.5. Compared to the omicron-fueled surge earlier this year, which caused case rates to peak quickly and fall sharply, the BA.5 surge has produced consistently high case rates over a longer period of time.
Dr. Noha Aboelata, CEO at Roots Community Health Center in East Oakland, said that COVID cases are “plateauing at a high rate, which you never want to see, of course.”
Symptoms caused by the new variant are believed to be similar to those we’ve come to expect from prior strains of COVID: fatigue, muscle pain, fever, coughing, headaches, sore throat and muscle pain, according to UC Davis Health.
Vaccinations, which have been found to minimize COVID symptoms, are fortunately high in Alameda County, where 86% of residents are fully vaccinated. The number is higher in Berkeley, at 94%, according to the Alameda County health department.
With case rates still high and questions swirling about BA.5 and other new variants, we’ve compiled some useful information about the current surge, the new variants, and where things stand on developing COVID treatments.
What to know
BA.5 is the most transmissible variant yet
Experts say BA.5, another iteration of the variant that caused the omicron surge, is the most transmissible subvariant yet. It makes up 78% of cases circulating in the United States. Here’s what you need to know about the latest subvariant:
“Every time you get a sub-variant, you get different mutations. What’s happening is that the mutations in BA.5 give it some special skills,” explained Dr. Kim Rhoads, an associate professor of epidemiology at the University of California San Francisco and the founding director of Umoja Health Partners.
In this case, BA.5 is more likely to evade immunity from prior infection. How long you are protected from immunity after an infection is shorter — a matter of three weeks instead of three months, give or take. Plus, the subvariant can be transmissible for longer, with more reports of people testing positive many days into their illness.
And the virus is continuing to mutate. The first case of BA 2.75, a new sub-variant that is driving another surge in India, was reported in the Bay Area on July 11, but little is known about it.
Case rates remain high
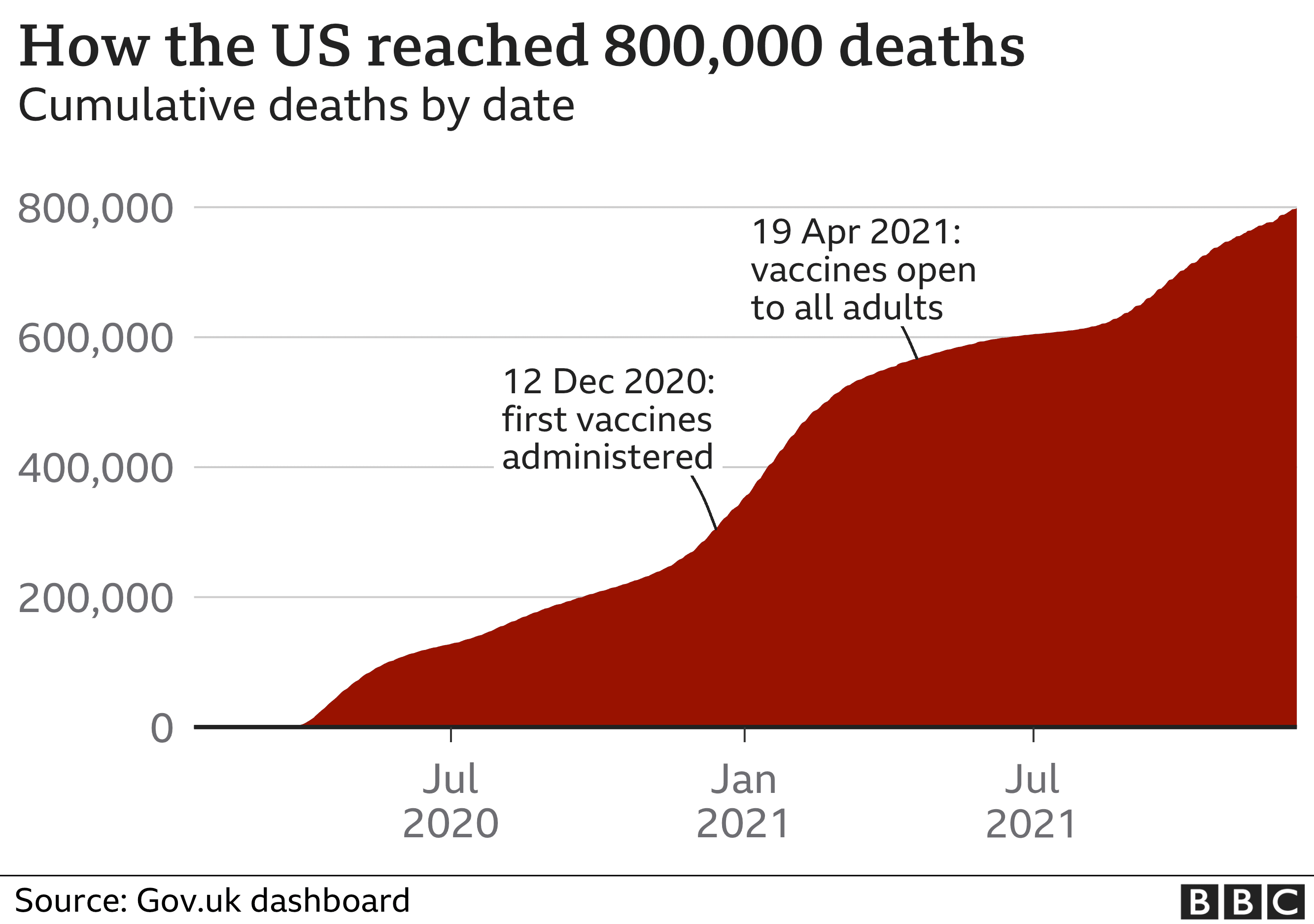
The latest surge has brought case rates in Alameda County to levels on par with the delta variant-fueled surge of early 2021 — although the true rate is probably much higher due to positive at-home tests that go unreported. Total daily cases across the county have hovered at around 1,000 for much of the past two months.
The Alameda County health department’s COVID dashboard shows the current surge reaching levels on par with delta in late 2020 and early 2021, but lasting longer. Source: Alameda County Department of Public Health
Last week, the case rate in Berkeley was 32 per 100,000 residents, compared with 181 cases per 100,000 residents in January. On average, there have been 34 reported cases each day in Berkeley in the last week.
As of July 21, the test-positivity rate is the highest it has been throughout the pandemic, at 10%. That’s in part because fewer people are getting tested, at least at testing sites — the number of people getting tested each day in Berkeley dipped below 500 per day last week — but Rhoads said the figure does reflect high levels of community spread.
Statewide, CDC data measuring the week of June 20 to June 26 shows that unvaccinated people 12 and over were more than 5.5 times likelier to contract COVID than their fully vaccinated counterparts. Similarly, unvaccinated people were over nine times more likely to be hospitalized and about eight times more likely to die than those who were fully vaccinated during this time period, when the sub-variant BA.5 was the most prominent form of the virus.
Wastewater tests suggest COVID levels continue to rise
Wastewater testing has proven to be a useful tool for gauging the rate of COVID infections in populations, as at-home tests create the possibility for positive results to go unreported.
The results from the wastewater tests, called an “early warning system” by the CDC, are often indicators of where reported cases and even hospitalizations may stand in the near future, as infectivity may be immediate but reported results or developing symptoms may take days.
The California Department of Health CDC wastewater monitoring site is experiencing some data delays for Alameda County. However, existing data from the two sewer sheds serving the county shows that COVID levels in our wastewater remain high — and infections are likely increasing.
Sewershed 137, which serves 740,000 people in Alameda and Contra Costa counties, shows steadily rising levels of virus in the wastewater.

A second, Sewershed 564, which serves a much smaller population of 60,000 residents in Alameda County alone, shows a fluctuation of COVID levels over the past two months, which may or may not be due to inconsistencies or delays in the water sampling there. We will update this data as we learn more.

Taken together, the data suggest that the current surge being driven by BA.5 is likely to continue at least into the near future.
Hospitalizations are up, but serious illnesses and deaths are still rare
Hospitalizations have been rising steadily, creeping upward in Alameda County since April, but serious illness remains largely limited to vulnerable groups, and unvaccinated and unboosted individuals are much more likely to be hospitalized with the virus.
There were 22 patients in the ICU in Alameda County and 142 in the hospital on July 14, still well below the number of people hospitalized during winter surges in 2021 and 2022.
At Stanford Hospital, 35% of patients who tested positive for COVID were hospitalized due to severe illness caused by the virus, while 65% were being treated for illnesses not related to COVID, according to The East Bay Times.
However, hospitalization numbers don’t necessarily reflect the risk of serious illness, since the risk of long COVID, still poorly understood, is not captured in those statistics.
Since the start of the pandemic, 62 people who died in Berkeley had COVID listed as a cause of death, the vast majority of whom were elderly. Two people under 51 years old with COVID have died in Berkeley and 14 have died between ages 51 and 70.
COVID treatments are more accessible than ever
In an interview, Dr. Aboelata (of Roots Community Health Center) spoke out against the common misconception that infected individuals should wait and see how bad their symptoms are before seeking treatment. Rather, those with higher risk factors such as being unvaccinated, being elderly, or having any of a long list of underlying conditions should seek treatment immediately after a positive test result.
Treatment itself has come a long way from the early pandemic, with an array of medications available at local pharmacies with costs covered by the federal government. Dr. Aboelata at Roots is a proponent of approved (or authorized for emergency use) outpatient treatments for people who become sick, with the oral antiviral medication Paxlovid being the first line of defense after infection. The intravenous broad-spectrum antiviral drug Remdesivir and intravenous monoclonal antibody treatments are also now available. Molnupiravir, which the FDA authorized in 2021 for mild-to-moderate cases, is the fourth treatment currently available.
“The monoclonal antibodies are actually so far holding up even against the BA.5 sub-variant,” said Aboelata. “We expect it to hold up well against [other] variants.”
Tried and true COVID-prevention measures are still recommended
To prevent the spread of the virus, doctors still recommend the same interventions, but they bear repeating. According to Rhoads, there remains a lot of misinformation about how the virus transmits.
“COVID is airborne. But we have everybody washing their hands, wiping off surfaces, and staying 6 feet apart,” Rhoads said. In reality, the most effective intervention against an airborne virus we have is wearing a mask.
To Rhoads, a more transmissible sub-variant warrants stepping up the safety precautions. She recommends avoiding crowded indoor places, including churches and dinner parties, where there are many people in attendance, wearing a mask in public, even outdoors, and getting tested often.
“Get comfortable. We’re just going to be in a mask for a bit,” Rhoads said.
Neither Berkeley nor Oakland now require people to wear masks indoors, although individual businesses or venues may still ask patrons to wear masks or provide proof of vaccination. In Berkeley Unified School District, masks are now “strongly recommended” but not required.