Why is mainland China sticking with “zero-COVID” policy?
Mainland China’s zero-Covid policy is increasingly unsuitable to
contain the much more infectious new coronavirus disease 2019
(COVID-19) variants, yet is likely to remain unchanged this
year.
The policy has exacted heavy tolls on the economy, as containing
outbreaks of the new variants requires extreme restrictions,
including citywide lockdowns. Zero-covid policy lockdowns in the
spring of 2022 caused disruptions to the Chinese economy not seen
since the severe economic contraction in the first quarter of 2020
owing to the initial Covid outbreak in Wuhan.
Hastily relinquished pandemic curbs could lead to large-scale
infections and death surges given the under-resourced medical
system and the large, insufficiently protected elderly population.
That would undermine Chinese Communist Party (CPC) leader Xi
Jinping’s repeated emphasis that “people and lives should come
first.”
Stringent lockdown measures could continue to be the “tool of
last resort” for a dynamically COVID-19-free environment throughout
2022. Near-term dependence on the “test and lockdown” approach
would at least help authorities to mitigate risks of a healthcare
crisis beyond what they are able to control.
Healthcare resource concerns
The strict pandemic responses – also supported by unparalleled
public obedience – have helped keep the domestic COVID-19 infection
count at extremely low levels and reduced disruptions to healthcare
service provisions unrelated to the pandemic. An abrupt relaxation
of the current policy would risk breaking the balance between
COVID-19 and non-COVID-19 healthcare needs and overstretching the
underdeveloped healthcare system.
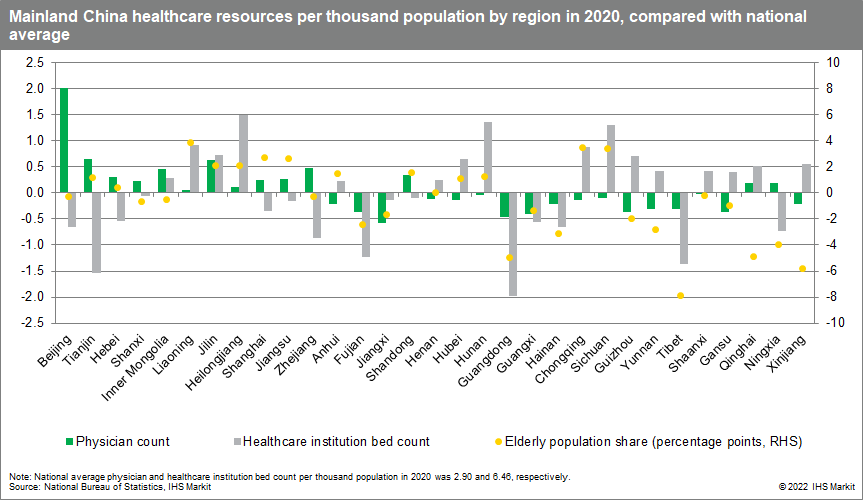
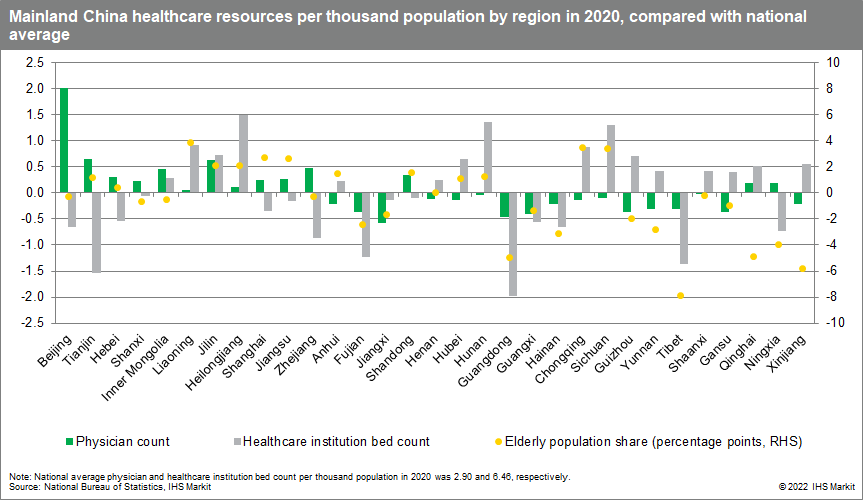
By the end of 2020, mainland China’s number of practicing
physicians reached 2.9 per thousand people compared with 2.6 in the
United States, and 4.4 for the OECD country average. The shortage
of nurses appeared more concerning, as China’s number of nurses per
thousand population was reported at 3.34 – far below the US level
of 12.0 and the OECD country average of 8.8.
China appeared better positioned in terms of medical
infrastructure, with 6.46 beds at healthcare institutions per
thousand people – higher than the level of 2.8 beds in the US, and
the OECD country average of 4.4 beds.
The healthcare systems across the regions have a “physician-hospital bed mismatch” issue – regions with a higher
physician count per thousand people may have insufficient hospital
beds, and vice versa.
More developed areas like the northern coastal region (Beijing,
Tianjin, and Hebei) and the eastern coastal region (Shanghai,
Jiangsu, and Zhejiang) have an above-national-average number of
physicians per thousand people, yet their hospital density is
falling behind.
Less developed regions like the southwest (Sichuan, Chongqing,
Guizhou, Yunnan, and Guangxi) and Midstream Yangtze River (Hunan,
Hubei, Anhui, and Jiangxi) on the contrary have more hospital beds
per thousand people than the national average but fewer
physicians.
Uneven regional distribution of people 65 and older is another
concern. The three northeastern provinces (Liaoning, Jilin, and
Heilongjiang) have both above-national-average numbers of
physicians and hospital beds per thousand people. They also have an
older population – the share of those aged 65 and above among the
local population is 2.9 percentage points higher than the national
average. This is likely to cause relatively greater stress on
healthcare resources amid any significant COVID-19 resurgence.
Vaccination factor
Vaccination is particularly crucial for China, because the
country’s extremely low Covid-19 infection rate indicates the
absence of natural immunity.
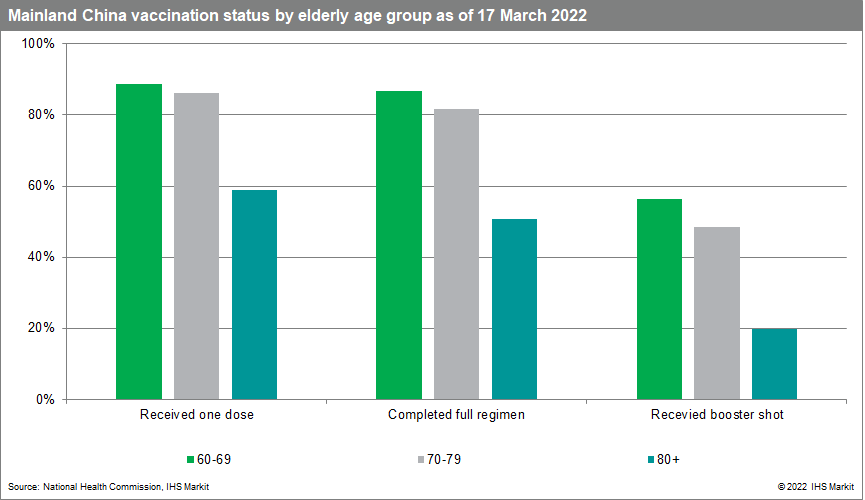
China has achieved a full vaccination rate of nearly 90% and a
booster shot coverage of approximately 55% among the entire
population. Vaccination progress among the elderly lags other age
groups, with hesitancy partially coming from underlying health
conditions, concerns over potential side effects, and the lack of
urgency owing to China’s early containment successes.
The latest release from China’s National Health Commission
suggests that the fully vaccinated share of the population has
reached 82.7% for people aged over 60 years, and only just exceeds
50% for those aged over 80.
At the regional level, reports on full vaccination progress for
the elderly population are limited. In mid-April, at the height of
Shanghai’s latest COVID-19 wave, 62% of the local population aged
above 60 years had reportedly completed a full vaccination regimen.
The share was just 15% for those above 80.
Concerns remain about the unclear efficacy of homegrown vaccines
deployed domestically. In contrast to developed economies that
widely use mRNA vaccines, mainland China has relied heavily on
two-dose inactivated vaccines manufactured by Sinopharm and
Sinovac. In addition, mainland China has approved the use of “mix
and match” booster shots since mid-February 2022 to enhance the
immune response.
A study jointly conducted by the University of Hong Kong and the
Chinese University of Hong Kong found that a third dose of mRNA
vaccine given to those who completed their primary inoculation with
two doses of either inactivated or mRNA vaccines can “provide
protective levels of protective antibody against the Omicron
variant,” while three doses of inactivated vaccines cannot provide “adequate levels of protective antibody.”1 Researchers remarked
that countries primarily using inactivated vaccines should consider
mRNA vaccine boosters to “achieve optimal protection against the
Omicron variant.”
Political considerations
With the 20th CPC Congress scheduled for the end of this year –
during which Xi is expected to secure an unprecedented third term
as leader of the CPC – it is likely that ensuring continuity in
policy, and wide buy-in from local governments on current
governance principles, will be the top priority at all costs.
A recent study by researchers at China’s Fudan University and
the US’s Indiana University validates Beijing’s hesitancy in
relinquishing zero-Covid policy.
The study simulated a scenario in which the Omicron outbreak in
Shanghai in March 2020 was allowed to evolve for six months without
non-pharmaceutical intervention (NPI) measures developed since the
2020 Wuhan outbreak (that is, removing the dynamic zero-COVID
policy).2 In this scenario, the outbreak would result in 112.2
million symptomatic cases, 5.1 million hospital admissions, 2.7
million ICU admissions, and 1.6 million deaths. At peak outbreak,
demand for ICU beds would reach 15.6 times national capacity. A
COVID-19 outbreak that leaves 1.6 million dead and overruns the
healthcare system would pose serious risks to social instability
and is thus politically intolerable.
Theoretically, introducing more effective foreign-made mRNA
vaccines would help to better protect the population against
COVID-19 variants. Chinese authorities have clear political reasons
to prefer domestic vaccines over foreign options. Relying on a
foreign vaccine supplier to establish domestic immunity could
potentially compromise national security. A domestic switch to a
foreign mRNA vaccine would also create negative political optics,
as more than 2 billion doses of homegrown vaccines had been
exported and donated overseas by the end of 2021.
Regardless, the rollout of a more effective vaccine – either
domestically or foreign made – would not fully prevent any fallout
from an exit wave of infections. This suggests that it would have a
rather limited impact on the general principle of dynamic
zero-COVID at the national level, as Xi’s policy for COVID-19
containment includes an extremely low level of infections.
Incentives for stringent pandemic control would be even stronger
at the local level, as any failure of COVID-19 containment would
threaten regional politicians’ careers far more than would an
economic slowdown.
Outlook for future easing
Any meaningful easing of the dynamic zero-COVID approach would
most likely be pushed back until 2023.
When the latest wave is farther in the rare view mirror,
attempts at more sustainable pandemic responses in favor of
commercial interests remain likely. This could be especially true
in areas where significant local lockdown fatigue undermines social
stability and business sentiment. Though actual implementation
would largely hinge on local pandemic situation, mid-tier coastal
cities like Ningbo City of Zhejiang Province, Xiamen City of Fujian
Province, as well as inland cities with stronger economic ties
overseas like Chengdu City of Sichuan Province, could be among the
top candidates to pilot easing, while keeping the risks at a
manageable level.
Possible relaxation measures could include reducing quarantine
requirements and adopting pilot programs in selected cities with
higher vaccination rates and relatively robust medical
capabilities.
The study of uncontrolled Omicron transmission by the
researchers at Fudan University and Indiana University also sheds
light on potential public health policies that could help to ease
the dynamic zero-COVID policy.
The study simulated the impact of Omicron-mitigating measures –
specifically, targeted vaccination of the population aged 60 and
older, and wider utilization of the Chinese government-approved
COVID-19 antiviral medications.
In vaccination simulation for people 60 and older, hospital
admissions were reduced by 33.8% from the baseline scenario to 3.4
million, ICU admissions were reduced by 54.1% from baseline to 1.2
million, and deaths were reduced by 60.8% from baseline to 0.6
million.
Wider use of antivirals resulted in a reduction in
hospitalizations ranging from 36.5% to 81.2% depending on the
medication regimen. A similar impact was seen on ICU admissions and
deaths.
Ideally, progress on the pharmaceutical front – such as more
widely accessible antiviral therapies or more effective vaccines –
would help to reduce the dependence on social and physical
distancing measures.
This article was published by S&P Global Market Intelligence and not by S&P Global Ratings, which is a separately managed division of S&P Global.