New BA.4, BA.5 coronavirus subvariants bypassing immunity
ALBANY — Over the last two years, New York has seen COVID-19 figures plummet in the summer months and then ramp up again in September when the weather cools and children return to school.
This summer is unfolding a bit differently due to a pair of highly contagious coronavirus omicron subvariants that are making the rounds in New York driving up infection and hospitalization rates across the state.
The subvariants called BA.4 and BA.5 now account for more than 50 percent of cases in New York, according to the most recent data from the Centers for Disease Control and the state Department of Health.
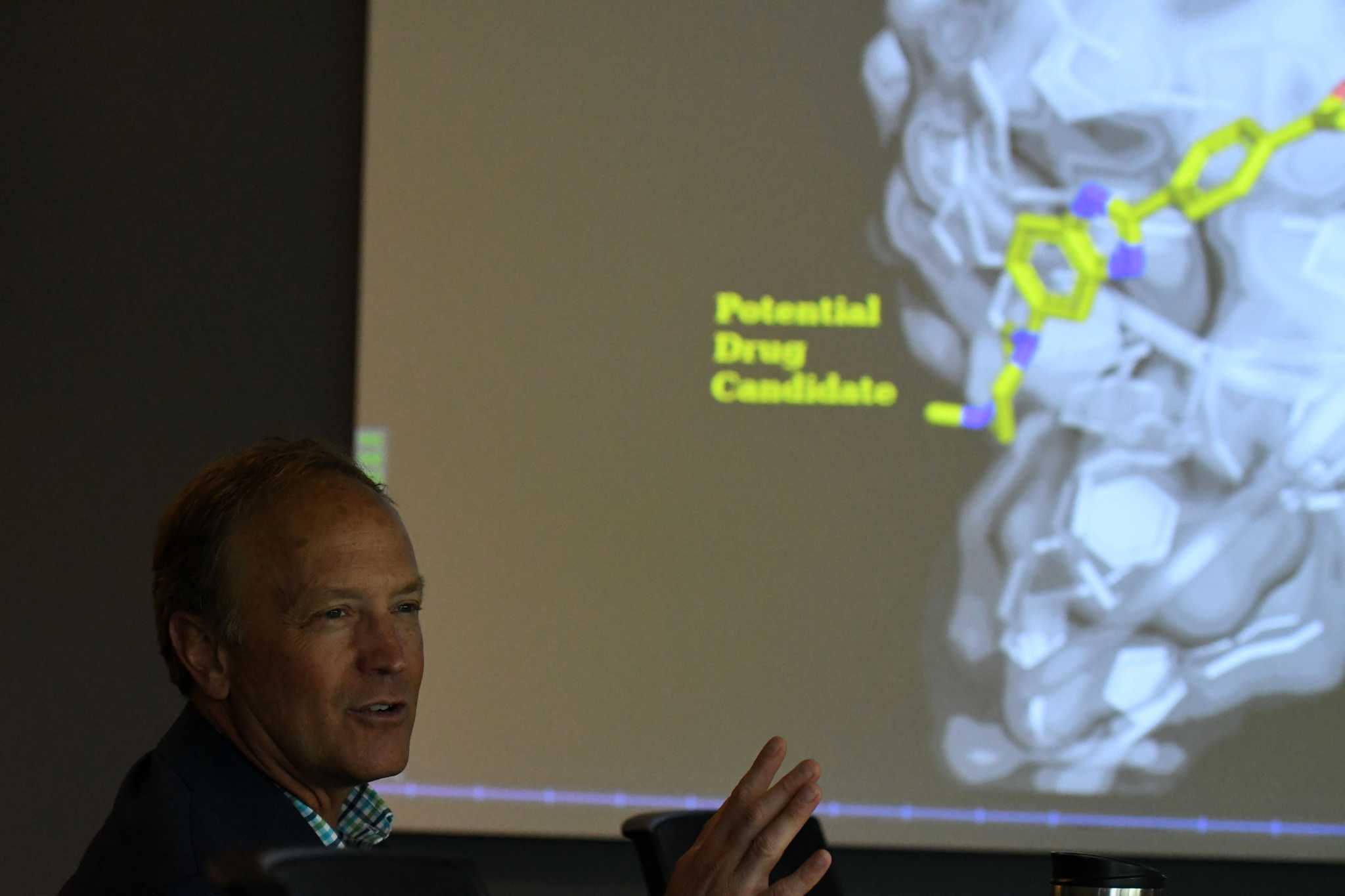
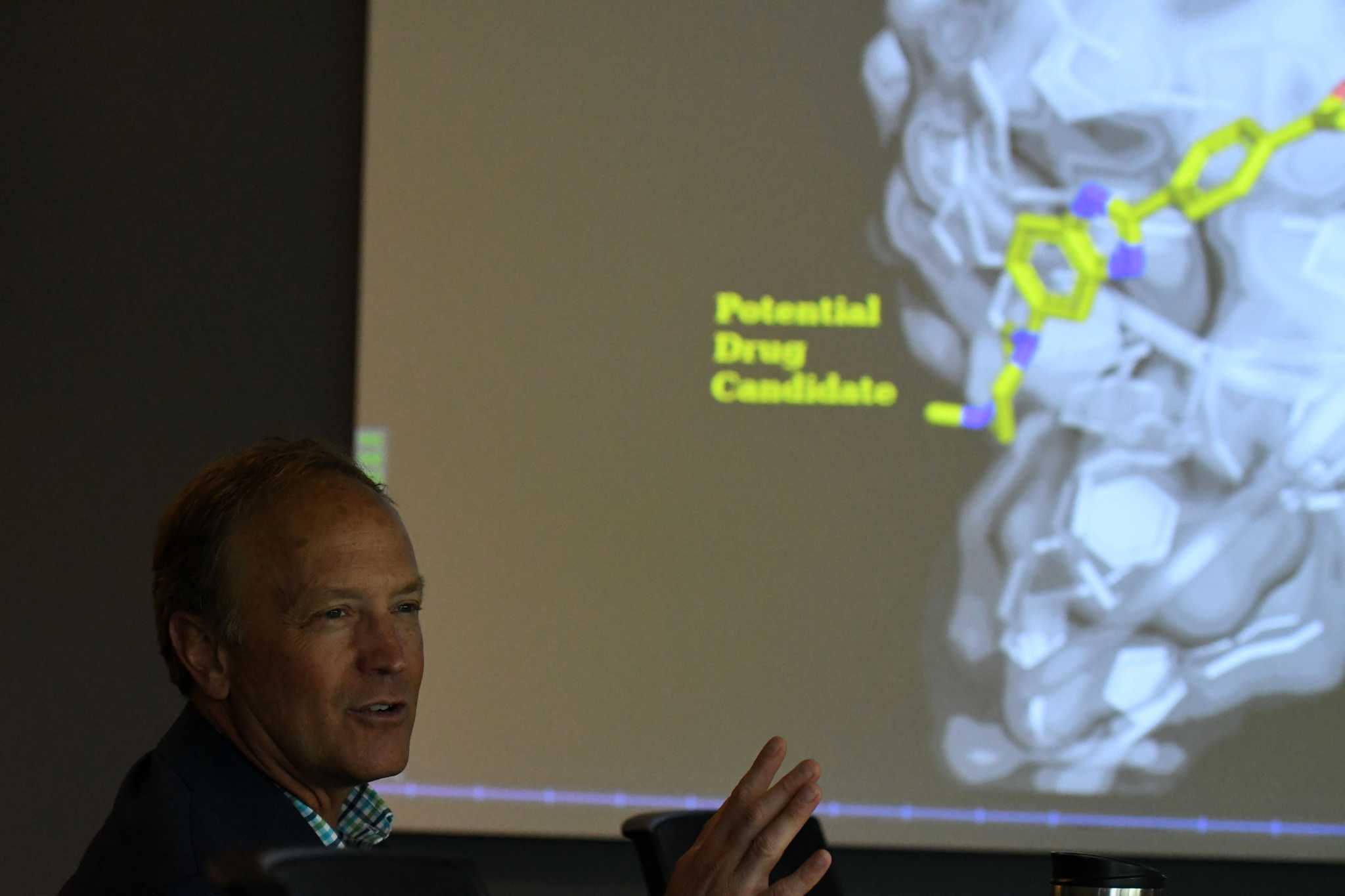
“Something that keeps impressing me is that the virus keeps getting more infectious,” said Dr. Andrew Berglund, director of the University at Albany (UAlbany) RNA Institute, which studies a variety of RNA-based diseases, including COVID-19 and myotonic muscular dystrophy.
RNA, or ribonucleic acid, is a single-stranded molecule found in the cells of living organisms that plays a critical role in protein creation among other cellular processes.
The RNA Institute’s genome sequencing lab is among those working with the state Department of Health’s Wadsworth Center Laboratory in Albany to analyze COVID-19 virus samples in order to identify current and emerging variants.
Berglund said that every time the SARS-CoV-2 virus (that’s the scientific name for the coronavirus responsible for the pandemic) replicates in a cell, it has a chance of mutating.
“Almost every person has a new variant … most of those mutations don’t mean anything. It sort of dies off with you, but when it’s a really good one, then it jumps,” he said. “What’s interesting about BA.4 and BA.5 is that the mutations are such that they are now evading the immune response that we have all built up.”
Genome sequencing has been around for decades but has become faster and more sophisticated in recent years, enabling scientists to track the tiniest mutations in the SARS-CoV2 virus.
From a public health perspective, RNA analysis is becoming more important as other metrics are less reliable indicators of an outbreak’s severity.
Earlier in the pandemic, health officials relied heavily on positivity rates in COVID-19 lab test results to determine how bad things were. The state DOH identified areas with clusters of disease and imposed restrictions for schools and businesses in those COVID-19 hotspots.
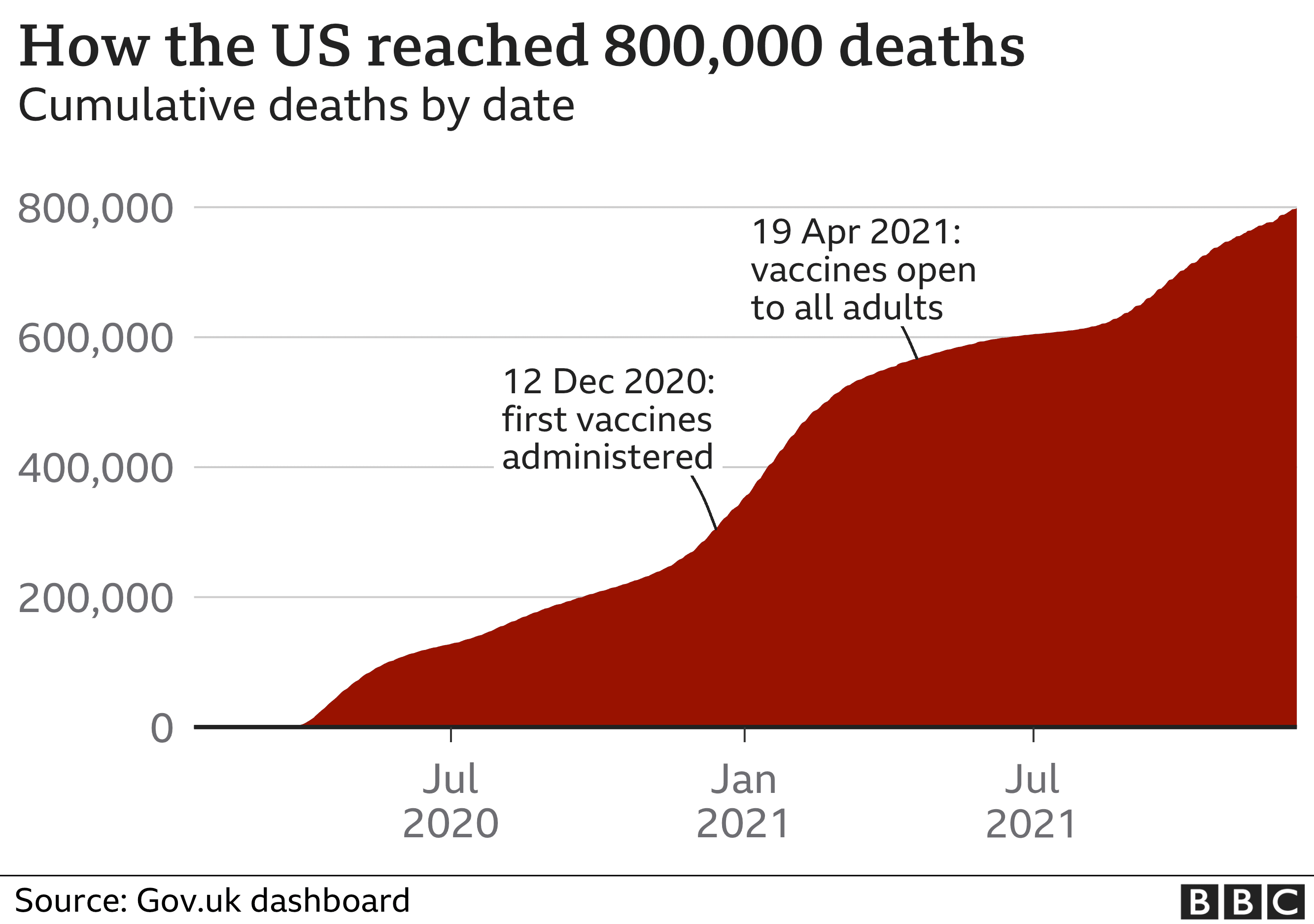
Now that untraceable at-home COVID-19 tests are commonplace, public health authorities say that cases are drastically undercounted. Hospitalizations and deaths are more accurate indicators, although those figures tend to lag behind infection rates.
COVID-19 hospitalization rates in New York are significantly higher this summer than they were around this time in 2020 and 2021.
On July 6 of 2020 and 2021, the hospitalization rate per population of 100,000 in New York was just over 4. On Wednesday, 11.5 per population of 100,000 New Yorkers were hospitalized with COVID-19, according to state Department of Health records.
In the Capital Region, current hospitalization rates paint an even starker picture when compared to the previous summer. Hospitalizations in the eight-county region are currently hovering at around 8 per 100,000 population, but at this time last summer, the hospitalization rate was at less than 1 per 100,000. Even on June 6, 2020, before there were vaccines available, the Capital Region’s hospitalization rate was at 2.21 per 100,000 people, according to state data.
State health officials said the elevated hospitalization numbers are associated with May’s COVID-19 surge which was largely driven by previous BA.2 subvariants, not BA.4 and BA.5. When case numbers increase, hospitalizations are likely to follow proportionately.
“We actively monitor COVID-19 statewide – including hospitalizations – and continue to urge New Yorkers to keep up with all recommended COVID-19 vaccine doses, their best protection against severe disease and hospitalization, as we know immunity wanes over time,” DOH spokesperson Sam Fuld said in an emailed statement.
RNA sequencing enables state health officials to anticipate the trajectory of the virus and adapt its public health strategy accordingly.
It also provides important data for drug companies like Pfizer and Moderna as they develop variant-specific vaccines.
The New York State Wastewater Surveillance Network is another vital data collection tool that will become more relevant as the pandemic evolves, state public health experts said. Sewage samples are collected and tested for the presence of COVID-19 multiple times a week in more than 90 sampling locations in 50 counties, with some counties already using it to notify residents of infection trends.
The state DOH continues to build out its wastewater surveillance testing system, and in the coming months, the program will be expanded to include sequencing of all SARS-CoV-2 positive water samples.
“This will facilitate the early detection of changes in circulating variants throughout that state, independent of clinical sample testing,” Fuld said.
Scientists are also working on new anti-viral therapies that can reduce the severity of the disease once someone is infected. Most COVID-19 treatments currently on the market must be administered early on in the disease or in a hospital setting.
Rensselaer Polytechnic Institute (RPI) researchers recently received a five-year, $3.5 million grant from the National Institute of Allergy and Infectious Diseases (NIAID) to help develop a low-dose, oral COVID antiviral drug that can be taken at home.
The virus may eventually lose its potency and die out, but a more likely scenario is that it will become endemic like the seasonal flu, which varies in severity each year, according to Berglund.
“COVID’s evolved,” Berglund said. “Our vaccines haven’t evolved yet, but they will.”