Can you get rebound COVID if don’t take the antiviral Paxlovid?
Can you get rebound COVID if don’t take the antiviral Paxlovid? San Francisco ChronicleView Full Coverage on Google News
Dear Advice Team: My husband and I both got COVID for the first time in late July, presumably from the highly infectious BA.5 variant. We are in our mid-60s, had our second booster in April, and are in good health overall. Because of our low risk situation, our physician did not recommend Paxlovid given the rebound issues.
We both developed the classic symptoms of sore throat, head congestion, fatigue, and body aches, along with mild fevers of a short duration at symptom onset — which was the same day for my husband as when Joe Biden first tested positive, and my symptoms started a day later.
I tested positive until day 15, and then tested positive again on day 17 after feeling symptoms worsen, and was back to testing negative again on day 18, though I’ve continued to have some symptoms (that have been much lighter over time). My rebound test sample was very bold and pronounced on day 17 after being progressively lighter for a few days before it first went negative.
At first we were feeling good about not taking Paxlovid when the president rebounded with a positive test, but then he ultimately tested negative sooner and was cleared earlier than both of us (and especially me with my longer duration). While the symptoms are fairly “mild,” they were uncomfortable and debilitating and I’m still not back and up to my regular exercise routine (at day 23). Perhaps if I had taken Paxlovid, I would have been feeling better much sooner and already back to my full exercise routine.
Send your questions and issues to pandemicproblems@sfchronicle.com.
We cannot respond to all questions, but your submission will be read and considered.
Please be as specific as possible, but try to keep it concise. We may edit your submission for space, clarity, or spelling and grammar.
Keep the people and situations in your letter anonymous by changing the names (including yours) and details. We will remove any identifying information.
Emails, letters, tweets or other messages you send become the property of The Chronicle and may be published online and in print.
Important: This column cannot address immediate risks to your health and safety. Call the National Suicide Prevention Lifeline at 800-273-8255 to reach a counselor at a locally operated crisis center 24 hours a day for free. Text “Connect” to 741741 to reach a crisis counselor any time for free.
Emails or other communications you send become the property of The Chronicle and may be published online and in print. By submitting a question, you agree to The Chronicle’s Terms of Use, which are available for review at sfchronicle.com/terms_of_use, and acknowledge its Privacy Notice, which is available for review at sfchronicle.com/privacy_policy.
The advice offered in this column is intended for informational purposes only. Use of this column is not intended to replace or substitute for any professional, financial, medical, legal or other professional advice. If you have specific concerns or a situation in which you require professional, psychological or medical help, you should consult with an appropriately trained and qualified specialist. The opinions or views expressed in this column are not intended to treat or diagnose; nor are they meant to replace the treatment and care that you may be receiving from a licensed professional, physician or mental health professional. This column, its authors, the newspaper and publisher are not responsible for the outcome or results of following any advice in any given situation. You, and only you, are completely responsible for your actions.
Given this apparent longer duration of COVID, does it make more sense to take Paxlovid?
Welcome to Pandemic Problems, an advice column that aims to help Bay Area residents solve their pandemic and post-pandemic conundrums — personal, practical or professional.
As COVID evolves into an endemic disease, we know readers are trying to navigate the “new normal.” Send your questions and issues to
pandemicproblems@sfchronicle.com
.
Today, The Chronicle’s Kellie Hwang fields an inquiry from someone who has suffered lingering COVID-19 symptoms and wonders whether they made the wrong call by not taking the antiviral drug Paxlovid due to “rebound” concerns.
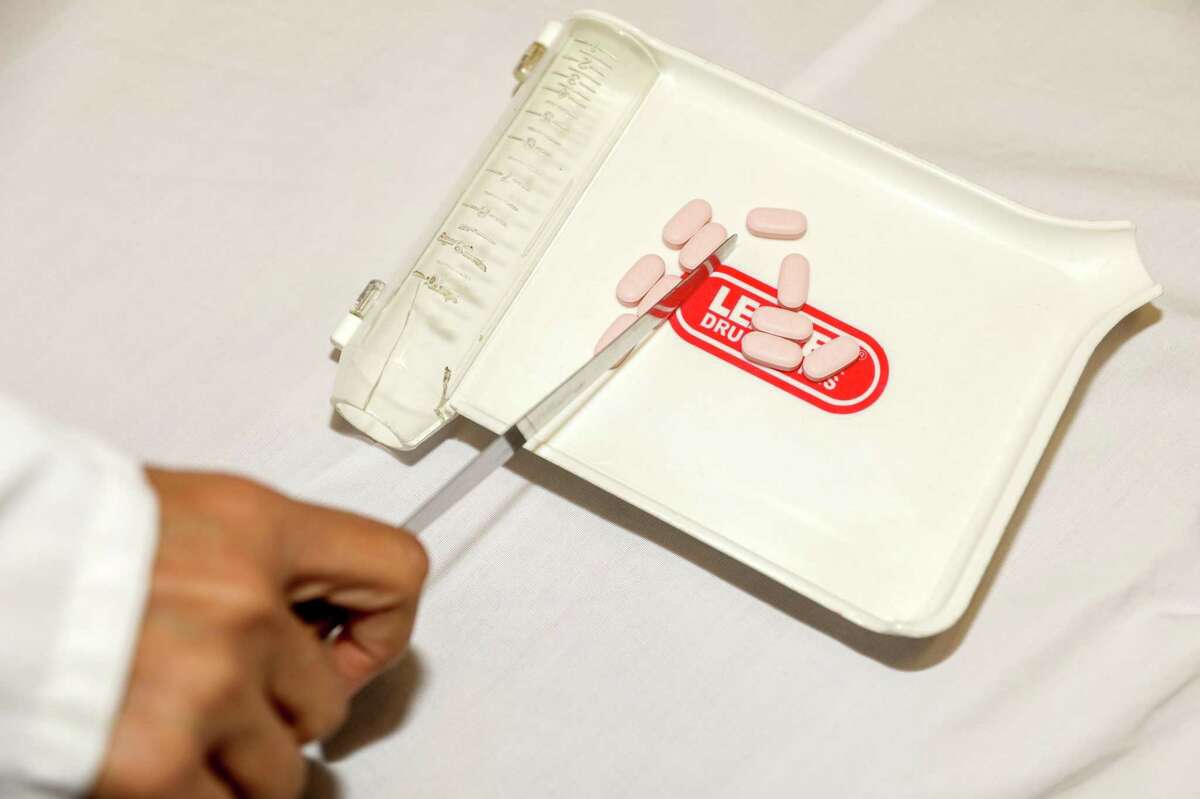
Dear Reader: Your questions revolve around the COVID-19 antiviral drug Paxlovid, so first, here’s some background for those unfamiliar with it: . The treatment consists of three tablets taken together twice daily for five days, for a total of 30 tablets, and the first dose must be started within the first five days of symptom onset.
Currently only people 12 and older who test positive for COVID and are at high risk for developing severe illness qualify for the prescription therapy. By default, this includes anyone over 50, or who is unvaccinated or has certain medical conditions.
In your case, you and your husband technically qualified for Paxlovid because you are both over 50. But you said your physician didn’t recommend the treatment because you are both lower-risk, given your vaccination status and overall good health, and also given the concern of possible Paxlovid “rebound” — which the CDC defines as completing the five-day treatment, and then developing COVID symptoms again, or testing positive again after a previous negative test.
It’s unclear how often such rebound cases occur among Paxlovid recipients — in clinical trials by the drug’s manufacturer, Pfizer, the phenomenon was reported in only 2% of patients, but anecdotal reports have been on the rise as the number of Americans taking Paxlovid has skyrocketed.
Now, on to your main question: Because you say you suffered a rebound of COVID-19 even without taking Paxlovid, you’re wondering whether the drug might have shortened the duration and severity of your illness — even if you had suffered Paxlovid rebound.
The short answer is that because so much research still needs to be done for both COVID-19 and Paxlovid, the experts I talked to can’t say definitively whether the therapy might have made a big difference in your case.
What is known, generally, is that people who are older and have medical conditions do benefit from taking Paxlovid, while younger people with or without conditions don’t seem to get much benefit.
Among higher risk patients, the drug has been found to significantly reduce the risk of hospitalization and death, according to Prasanna Jagannathan, an infectious disease specialist at Stanford.
A Pfizer trial conducted before the spread of the omicron coronavirus variant found that it “significantly reduced virus levels compared to placebo,” Jagannathan said, and reduced the risk of COVID hospitalization or death by 89%.
However, in a similar trial in lower-risk individuals, “Paxlovid was not found to significantly reduce the duration of symptoms or the risk of hospitalization or death, although it was shown to reduce virus levels in lower risk individuals as well,” Jagannathan said.
A recent study out of Israel after omicron became the dominant strain (BA.5, which you think you contracted, is an omicron subvariant) found that in individuals 65 and older, “rates of hospitalization and death due to COVID-19 were significantly lower among those who received Paxlovid than among those who did not,” Jagannathan said. In patients 65 and older, the risk of hospitalization was 14.7 cases per 100,000 in those who took Paxlovid, versus 58.9 cases per 100,000 in untreated patients.
But the study also found taking Paxlovid didn’t make any difference for younger patients with underlying conditions: In those 40 to 64 years old, the case rate was nearly the same in those who took Paxlovid versus those who did not.
Bottom line? “Regarding the reader’s question, I think it still makes sense to take Paxlovid if you are at higher risk of disease progression,” Jagannathan said. However, “For those at lower risk, although Paxlovid likely would significantly reduce virus levels, the evidence thus far does not suggest a large clinical benefit,” such as reduced risk of hospitalization or death, he said.
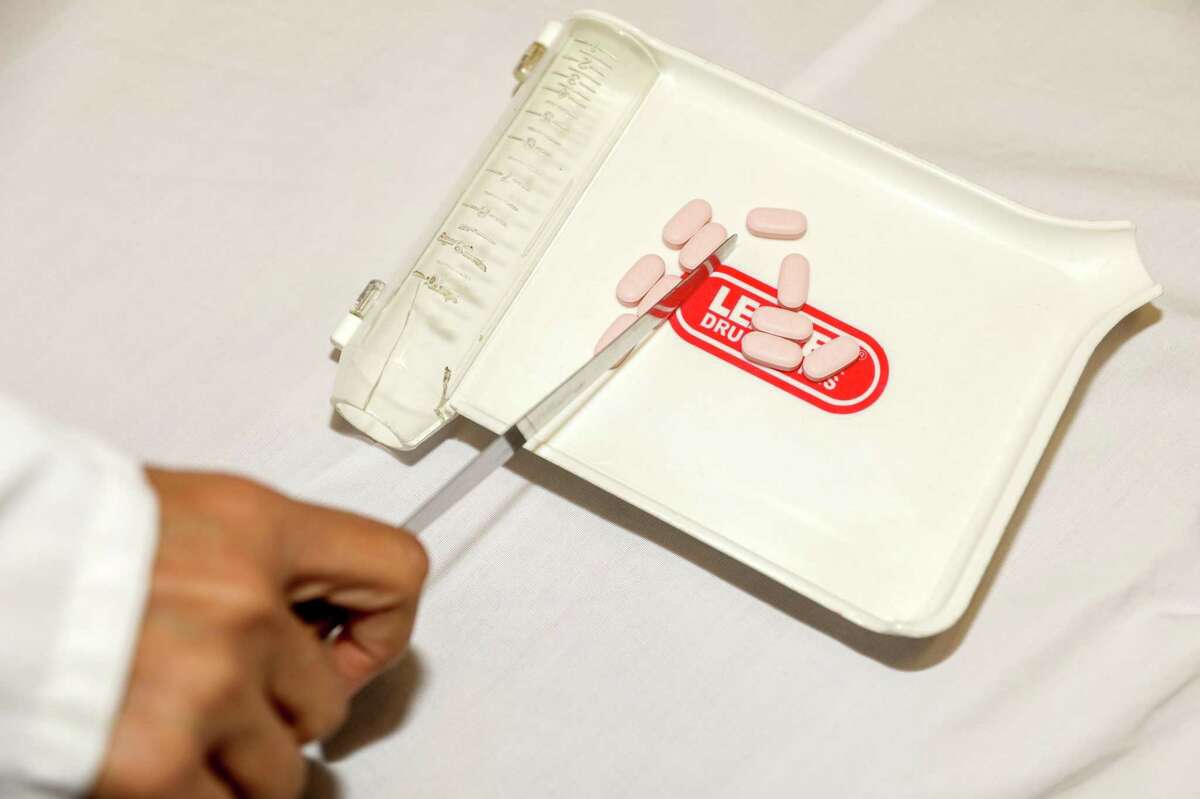
A reader who suffered lingering COVID-19 symptoms is second-guessing the decision not to take the antiviral drug Paxlovid because of rebound concerns.
Brontë Wittpenn/The Chronicle
Sarah Doernberg, an infectious disease expert at UCSF, echoed these remarks.
“For high-risk patients, there is a clear benefit to the drug,” she said. “For patients who may qualify at high-risk but have fewer comorbidities, are younger, are vaccinated, or otherwise are at lower risk for disease progression, the benefit may be less obvious.”
As you mentioned, President Joe Biden is a good example of someone in the high-risk category, along with his chief medical adviser, Dr. Anthony Fauci. At ages 79 and 81, respectively, both are well within the age group for whom Paxlovid is recommended. Both took it and suffered rebound after they had recovered from COVID and initially tested negative.
Regarding rebound, experts are still trying to get to the bottom of the phenomenon. It can occur in COVID patients who took Paxlovid, like Biden and Fauci, and those who didn’t, like yourself, and the degree of rebound risk for either group is still unclear, Jagannathan said.
Doctors interviewed by The Chronicle in June said anecdotal reports of Paxlovid rebound haven’t changed their opinion that for high-risk patients: The overall benefit still outweighs the risk, they said, and all rebound cases ultimately seem to resolve without patients needing hospitalization.
The medical community is still waiting for “rigorous and well-done studies” to find out if the rebound effect is specific to Paxlovid, if there’s anything that can prevent it from happening, and if any intervention is necessary, Doernberg said.
“At this point, there is a lot of speculation but not a lot of well-done studies to answer these questions,” she said.
One silver lining is that, unlike during the initial infection, the risk of disease progression during the rebound period is very low, Jagannathan said, “although individuals should be assumed to be infectious and should isolate.”
You didn’t mention that you had any concerns about Paxlovid side effects, and the clinical trials didn’t show any serious ones, Jagannathan said, but some patients develop a temporary bitter or metallic taste after taking the pills. The Federal Drug Administration lists diarrhea, increased blood pressure, myalgia, allergic reactions, abdominal pain and nausea as possible side effects.
Also, prescribers need to consider many important drug interactions, Jagannathan said. “Paxlovid is not recommended in patients with severe kidney impairment or in patients with severe liver impairment,” he said.
Pandemic Problems is written by Chronicle Advice Team members Annie Vainshtein and Kellie Hwang, combining thorough reporting and guidance from Bay Area experts to help get answers and find a way forward.