A population-based serological study of post-COVID syndrome prevalence and risk factors in children and adolescents
Our results showed that a significant proportion of children and adolescents suffered from persistent symptoms compatible with post-COVID syndrome. The overall estimated prevalence in the pediatric population was about 4%. Stratifying per age group, only adolescents displayed a substantial risk of having post-COVID symptoms. Risk factors for post-COVID syndrome were older age, having a lower socioeconomic status and suffering from chronic health conditions, especially asthma.
We defined post-COVID syndrome in children based on the recent definition published by Stephenson et al. in March 20223. The estimated overall prevalence of post-COVID syndrome in our sample is high, yet lower than in other studies4. There might be multiple reasons. First, designs, samples and characteristics of post-COVID varied considerably across studies. Second, our data included mildly symptomatic and asymptomatic children and, therefore, a greater number of infected children than when relying on confirmed infection alone as testing was never systematic in children. Third, we worked with a population-based sample rather than clinical registries. Finally, a proportion of seropositive children in our sample might have been infected too recently making it impossible to studied long term persistent symptoms.
Our data showed a meaningful difference in prevalence between children >12 years and younger individuals, in agreement with the study by Stephenson et al.5 We could expect this proportion to be higher in reality as parents might not be aware of all of their children’s symptoms; adolescents may be less open about their issues since they are in a period of their life seeking more independence.
The prevalence difference between seronegatives and seropositives (~8%) in adolescents is worth investigating as it potentially represents a very high absolute number, although lower than in adults11. Post-COVID syndrome might worsen adolescents’ lives, already negatively impacted by the general pandemic environment12,13 and could exacerbate long-term negative consequences on health, social and academic outcomes. On the contrary, we did not observe significant differences between seronegative and seropositive children <12 years14. The lack of difference in reported persistent symptoms in children <12 years could be partly explained by the relatively small sample size and by symptoms often developed after common respiratory infections other than SARS-CoV-2 in this age range.
The pandemic-related difficulties to meet psychological and physical developmental needs may have been exacerbated by persistent symptoms, further preventing children from going about their daily activities and worsening their mental health. Most declared persistent symptoms among seropositives were abdominal pain, trouble concentrating, smell loss, dripping nose, muscle pain, breathing difficulties, headache and constipation, in agreement with the recent literature4,15,16. The severity of symptoms reported by parents was, on average, slightly higher in seropositive children, suggesting that persistent symptoms following a SARS-CoV-2 infection might be more severe and represent a more substantial burden on their daily life14,17. Sher et al. underlined that depressive symptoms appear to be common in patients with post-COVID syndrome. Long-term medical and psychological consequences of post-COVID syndrome could drastically worsen mental health and even increase suicidal ideation and behaviors18. Similar outcomes could be expected in the pediatric population, especially in adolescents. Post-COVID syndrome should not be underestimated in children and calls for appropriate medical strategies including reinforcing vaccination strategies19.
In an analysis restricted to seropositives, children from households with lower socioeconomic status were more likely to experience post-COVID syndrome. This is in line with the growing literature on health inequalities of the COVID-19 pandemic in terms of incidence, testing and severity of the infection20. Those inequalities could be explained by differential exposure to the virus, greater susceptibility to infection, stronger comorbidities in vulnerable groups associated with severe outcomes, and disparities in healthcare. Similar mechanisms could explain the greater exposure of vulnerable children to the post-COVID syndrome. Also, it is reasonable to highlight that COVID-19 vaccination uptake was more frequent among individuals with higher socioeconomic status and is considered as the major protection against an acute or severe SARS-CoV-2 infection, hence developing a post-COVID syndrome21.
In our sample, post-COVID seems more prevalent among children with chronic disease, especially asthma, although causality could be bi-directional. In general, asthmatic children have a higher risk of respiratory infections. However, the association between asthma and SARS-CoV-2 infection remains unclear in the pediatric population, as many large-scale ecological studies presented reduced pediatric asthma during the pandemic likely due to physical distancing, masks, and perhaps decreases in air pollution. On the other hand, other research focused on the individual level and presented asthma as a risk factor for hospitalization in children with COVID-19, but not for worse COVID-19 outcomes22,23.
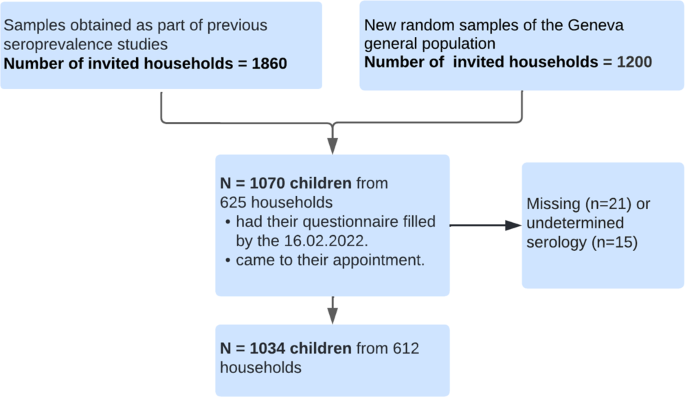
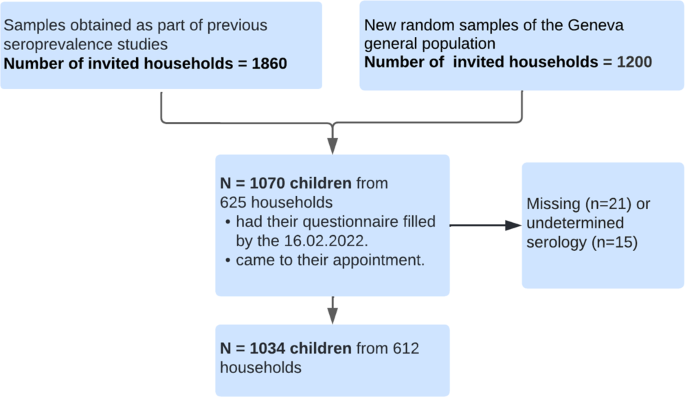
The major strength of our study is the population-based design with a wide age range, covering from babies to adolescents. Only very few studies on post-COVID syndrome rely on random population samples and include children of this age range4. We identified previous SARS-CoV-2 infections relying on serological data, which also detects previous asymptomatic and mild infection. Unlike studies relying on test-confirmed infections, which suffer from selection bias, relying on serological assessment yields a better estimation of the proportion of the infected population.
However, the use of serological data also poses challenges. In particular, it is impossible to determine the exact date of infection only relying on this data5. Our estimates are therefore based on a comparison of children with and without anti-SARS-CoV-2 antibodies, using a control group to avoid overestimating the prevalence of post-COVID symptoms. Although the diagnosis of post-COVID condition related to persistent symptoms could not be medically assessed by excluding all other alternative diagnoses, the comparison between seropositive and seronegative children enabled to control for the occurrence of persistent symptoms unrelated to a SARS-CoV-2 infection. Once again, this highlights the importance of a control group and the complexity of identifying the post-COVID syndrome methodologically and clinically. Furthermore, despite the fact that some parents were probably aware of their children’s exposure status when answering the questionnaire due to confirmed COVID-19 diagnosis or a symptomatic infection, relying on serological tests mitigates the bias of parents over-reporting persistent symptoms when knowing their child(ren) had been infected24.
Our study also has several limitations. Data were parent-reported and their answers could be influenced by their own experience or the household environment. Also, they might not be aware of some of their children’s symptoms, particularly for adolescents. Furthermore, as the time of infection and the date of onset persistent symptoms were unknown in many cases, we are not able to study the incident risk of post-COVID, for which another study design including the time of the infection and a follow-up would be necessary. Moreover, we cannot exclude that some children might suffer from long-lasting symptoms due to Omicron infection but were not identified as such in our analysis as they had not reached the 12-week threshold that we used to define persistent symptoms. This could have led to an underestimation of the prevalence of post-COVID.
Despite the high number of randomly recruited children from a wide age range, the participation rate was relatively low, although in line with participations rates in children cohort in other countries25. In addition to the general challenge of recruiting children in population-based cohort26, we faced the additional difficulty that parents were often reluctant to have their children, especially young ones, undergo a blood draw for research purposes only. We also noticed that some parents were tired of hearing about the pandemic, which also represented a strong barrier to recruitment. Finally, individuals with favorable socio-economic conditions were more likely to participate. This could have led to an underestimation of the prevalence of post-COVID since their occurrence was more common among underprivileged individuals. Overall, this might limit the representativeness of our results.
It would be interesting to study persistent symptoms in children and adolescents who were more recently affected with the Omicron variant as less virulent variants could potentially lead to lower prevalence of post-COVID.
Our study contributes to a better understanding of post-COVID in the pediatric population. The impact of COVID-19 vaccination could not be assessed and further studies should explore if prior vaccination reduces the risk of developing post-COVID.
A significant proportion of children experienced post-COVID symptoms lasting over 12 weeks after infection with an estimated prevalence of 4% overall and 8% in adolescents. Older age, having a chronic condition and living on a household with lower socioeconomic conditions were identified as risk factors for the post-COVID syndrome. Our understanding of post-COVID syndrome will likely evolve as scientific evidence grows. Nevertheless, it is fundamental to rapidly implement effective primary care management, including early screening and detection, and health promotion to assist children and adolescents suffering from this syndrome who might experience long term physical and mental adverse consequences.



